-Helminth Infestations-
-Helminths are multicellular parasites that have complex life cycles within and outside human hosts
-Anti-helminth drugs are used for treatment of symptomatic patients and deworming in regions with a higher prevalence of disease
-There are 3 man in groups of helminths: flatworms (platyhelminths), thorny headed worms (acanthocephalins), and round worms (nematodes)
-Flatworms include flukes (trematodes) and tapeworms
-Thorny headed worms reside in the GI tract
-Round worms can reside in the GI tract, blood, lymphatic system, and subcutaneous tissue. These organisms are not typically considered parasites
-Most intestinal flukes are asymptomatic. When symptoms occur can include inflammation, ulceration, and small abscesses in the intestine. Can get anorexia, nausea, vomiting, diarrhea and abdominal pain. Malabsorption can sometimes occur
-Diagnosis is made by observation of worms or eggs in stool or body fluids
-Treatment of intestinal flukes are Praziquantel
-Intestinal tapeworms when cause symptoms and patients note segments in their stool or movement through their anus. Patients may have nausea, anorexia, and epigastric abdominal pain.
-Diagnosis of intestinal tapeworms is made by visualization of the eggs or segments in their stool.
-Praziquantel is the treatment of choice for intestinal tapeworms
-Mebendazole is indicated for eosinophil colitis, anisakiasis, acariasis, capillarasis, larval tissue, pinworms, and hookworms
-Malaria-
-Malaria is caused by the plasmodia species (five different types)
-Most deaths that occur from malaria are from the plasmodia falciparum species
-Incubation period can be 12-35 days depending on the species
-The next step is the erythrocytic stage where there is a release of merozoites from the infected red cells when they rupture that causes fever and other manifestations
-Malaria should be suspected in any patient with a fever who has had an exposure to a region where malaria is prevalent
-Symptoms are non specific and may include fever, chills, tachycardia, tachypnea, malaise, diaphoresis, headache, cough, anorexia, nausea, vomiting, abdominal pain, and myalgias
-Physical exam may reveal anemia with splenomegaly
-Patients with complicated malaria may have altered LOC, seizures, ARDS, shock, metabolic acidosis, renal failure, liver failure, DIC, severe anemia, hypoglycemia, and massive intravascular hemolysis
-Diagnosis is made by blood smear or rapid diagnostic test.
-Treatment for uncomplicated malaria includes:
1. Artermisinin derivative combinations
2. Malarone
3. Quinine in combination with doxycycline or clindamycin
4. Lariam in combination with artesunate or doxycycline
-Two major classes available for parenteral treatment for severe malaria quinine and artemisinin derivatives
-Pinworms-
-Enterobius vermicularis (pinworms) is one of the most common nematode infections worldwide
-The cycle beings when female worms deposit themselves on perianal folds
-Autoinfection occurs by scratching the perianal area and transferring infective eggs to the mouth and contaminated hands
-Person to person spreading is done by contact
-After ingestion, eggs hatch and release larvae in the small intestine. Gravid females migrate to rectum and and deposit eggs usually at night
-Most of the time infection is asymptomatic, may get peri-rectal itching and excoriation
-Diagnosis is made by the scotch tape test where clear tape is applied against the perennial skin allowing the eggs to adhere to the tape. May see via gross examination
-Treatment is with albendazole or mebendazole once and repeated in 2 weeks
-Toxoplasmosis-
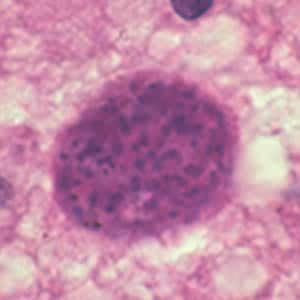
-Toxoplasmosis is an infection caused by an intracellular parasite
-Toxoplasma gondii is the organism that causes toxoplasmosis
-Immunocompetent patients typically are asymptomatic with primary infection
-If those patients become immunocompromised, they may exhibit only mild symptoms initially
-Felines are the only animals Toxoplasma gondii can complete its reproductive cycle
-When humans ingest T. Gondii eggs the organisms invade the intestinal epithelium and disseminate throughout the body
-There are many ways of acquiring toxoplasmosis in humans:
1. Ingestion of infected oocytes from the environment
2. Ingestion of tissue cysts in meat form an infected animal or contaminated fruits and vegetables
3. Can be based from an infected mother to fetus
4. Can be transmitted by blood or organ transplantation from donor
-When immunocompetent patients are infected with toxoplasmosis patients usually have bilateral symmetrical non tender cervical lymphadenopathy. May also have generalized lymphadenopathy, fever, chills, sweats, myalgias, pharyngitis, non pruritic maculopapular rash, or hepatosplenomegaly
-Most immunocompetent patients have benign self limiting course lasting weeks to months
-T. gondii is the most common pathogens to cause chorioretinitis (posterior uveitis)
-ELISA serology is the most common diagnostic test employed for diagnosing toxoplasmosis
-Immunocompetent, non pregnant people do not require treatment unless symptomatic for over a month.
-Patients with AIDS with low CD4 counts can have reactivation of the disease easier and become quite ill.
-When Toxoplasmosis reactivates in AIDS patients it most commonly does so causing CNS encephalitis, and leads to cerebral abscesses
-Other areas of the body affected with toxoplasmosis is immunodeficient patients include pneumonitis and chorioretinitis
-Pregnant women who experience a mono like illness and have a negative test should be screened for toxoplasmosis
-The risk of fetal infection increases steeply with advancing gestational age at the time of maternal seroconversion
-A prenatal diagnosis requires an amniocentesis. Risks versus benefits have to be outweighed
-Treatment of Toxoplasmosis is accomplished with pyrimethamine plus sulfadiazine or clindamycin
-Leucovorin should be given to all patients with pyrimethamine (for the folic acid)
-Treatment is typically at least 6 weeks for those who respond to treatment


No comments:
Post a Comment